- Introduction Of Enhancing Cardiovascular Care Professional Assignment
- Recent diagnosis of coronary heart disease
- Pathophysiology of CHD and Risk Assessment
- Patient Assessment and Care Planning
- Challenges in Risk Factor Control
- National and Local Guidelines for CHD Diagnosis and Management
- Pharmacological and Non-Pharmacological Approaches
- Reflection on Best Practices and Ethical Considerations
- Personal Reflection on My Learning Journey
- Conclusion
Introduction Of Enhancing Cardiovascular Care Professional Assignment
British people lose their lives and fall ill because of cardiovascular disease (CVD), which takes around 160,000 patients each year, while coronary heart disease (CHD) results in 66,000 deaths yearly (Tidy, 2022). CHD exists as an illness affecting 2.3 million UK citizens, and doctors expect these numbers to grow because obesity, diabetes, and inactive lifestyles become more common. The NHS Long-Term Plan identifies early testing, lifestyle changes, and medication treatment as fundamental measures to lower CHD medical burden and enhance patient recovery results (NHS England, 2014). This study tracks the experience of a new CHD patient through an evaluation of risk assessment combined with treatment interventions and national healthcare guidelines used for condition management.
Recent diagnosis of coronary heart disease
The biopsychosocial assessment reveals medical problems, behavioural patterns, and socioeconomic elements, determining how well the patient follows the treatment. Research data from the UK shows that 67% of men, along with 13.3% of adults who smoke, make up the country's obesity and smoking statistics. Proper structured medical interventions by different healthcare specialists are vital to boost medical outcomes and minimise the chance of heart problems (Afik et al., 2022).
It is a 58 male who was recently having an episode of exertional angina, an essential sign of underlying coronary artery disease. High blood pressure, elevated cholesterol, obesity and a long history of smoking are part of the medical history. They also live a predominantly inactive lifestyle and work too much and too hard. The patient’s family background also amplifies cardiovascular risks significantly if someone in the family also has coronary disease. Taking into account their medical history and current lifestyle habits, one of the categories that put them at high risk for cardiovascular events. The second point includes a complete biopsychosocial evaluation. Furthermore, it points out that physical issues do not always influence the person’s response to treatment. Moreover, they also influence social circumstances, mental health, and the availability of healthcare resources (Hamrahian et al., 2022). The UK has high obesity rates, and national data also highlights how difficult it is to combat the persistence of smoking despite such efforts.
Need Assignment Help that delivers results? Trusted Assignment Help in UK for well-researched, plagiarism-free academic solutions.
Pathophysiology of CHD and Risk Assessment
Atherosclerosis, a progressive disease resulting in the accumulation of fatty deposits within the coronary arteries, plaque formation, and vascular inflammation that leads to reduced oxygen supply to the myocardium, is the cause of CHD development (Pursnani and Merchant, 2020). Endothelial dysfunction, dyslipidaemia, hypertension and oxidative stress are the main factors promoting this pathophysiological process. Plaque rupture can lead to acute coronary syndromes such as myocardial infarction, which are responsible for a large number of emergency hospital admissions in the UK as the disease progresses (Ewelina Młynarska et al., 2024). In clinical practice, many patients are risk stratified using risk stratification tools like the QRISK3 calculator or Framingham risk score to evaluate a patient’s chance of developing CHD in 10 years. PHE data indicates that some 7.6 million people are living in the UK with heart and circulatory diseases, and it is vital, the data says, that we identify people at risk early and take steps to prevent this, starting with prevention (Ewelina Młynarska et al., 2024).
Most often, coronary heart disease is caused by atherosclerosis, when fatty plaques accumulate in the coronary arteries, cutting the blood vessels and reducing the blood flow to the heart muscle. This is a function of elevated cholesterol, high blood pressure and oxidative damage to the blood vessel linings (Mehta, 2024). The plaques can rupture as the disease progresses, and this can result in acute coronary syndromes, such as a heart attack. It is essential to identify early individuals at risk for later intervention. In clinical settings, risk assessment tools such as QRISK3 and Framingham Risk Score are commonly used to predict whether a patient is at risk of having a cardiovascular event soon (Thibaut, 2018). Early screening, prevention and management of cardiovascular diseases is recognized as a national and global health policy priority with the WHO Global Noncommunicable Diseases Action Plan and NMHS Long Term Plan.
Patient Assessment and Care Planning
Patient assessment requires an integration of clinical history, lifestyle factors and diagnostic tests to create a patient-specific management practice. Cardiac function and vascular health are evaluated by electrocardiography (ECG), echocardiography, lipid profile analysis, and ambulatory blood pressure monitoring. It follows the approach used by NICE NG185 guidelines based on a person-centred care model, which matches the intervention with the patient’s values, preferences and socioeconomic situation (NICE, 2020). If this test is positive, a multidisciplinary team of general practitioners, cardiologists, dietitians, and physiotherapists, with the addition of a nurse, consolidates the data to develop a specialised care plan based on smoking cessation, change in diet, pharmacological therapy and structured physical activity. As stated by Toukhsati et al. (2019) patient participation in self-care interventions greatly improves treatment adherence. Based on studies, patients going to cardiac rehabilitation programs have 30% fewer incidences of readmissions to hospitals than patients not in these programs. Healthcare professionals can adapt behavioural change models such as motivational interviewing and cognitive behavioural therapy (CBT) to increase patient engagement in chronic cardiovascular risk reduction strategies and long-term adherence.
An adequate medical history of patients, risk factors, and lifestyle choices will allow a healthcare professional to manage the patient’s condition (Nichol et al., 2024). The assessment of the heart function and the status of the heart and the vascular system included diagnostic tests, such as electrocardiograms (ECG), echocardiography, cholesterol, screening and 24-hour blood pressure measurement. To follow, dependent on the patient's preferences and circumstantial life, a personalized care plan that fits their situation is recommended by national guidelines (Parreira et al., 2021). This team of cardiologists, general practitioners, nutritionists, and physiotherapists meet to make a lifestyle change plan, including smoking cessation, feeding adjustments, and exercise. Evidence exists that involving patients in structured self-care programs, like cardiac rehabilitation, can improve adherence to the treatment and reduce readmission rates. Behavioural change models such as motivational interviewing help instil the patient in their treatment and long-term heart health.
Challenges in Risk Factor Control
Despite advancements in screening and early detection, the management of CHD is often complicated by poor risk factor control. Smoking cessation remains a significant challenge, with 13.3% of UK adults still smoking, leading to an estimated 74,600 smoking-related deaths annually (Office for Health Improvement & Disparities, 2022). Similarly, over 27% of UK adults are classified as obese, significantly increasing the risk of metabolic syndrome and cardiovascular complications (Powell-Wiley et al., 2021). Non-adherence to lifestyle modifications and prescribed medications is another critical barrier, influenced by low health literacy, socioeconomic deprivation, and psychological resistance to change.
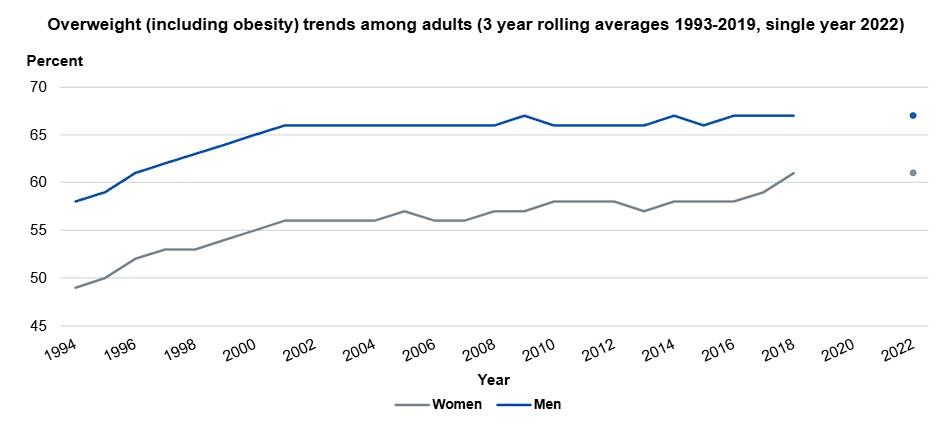
Figure 1: Health Survey for England, 2022 Part 2
The effectiveness of lipid-lowering interventions is reduced, as studies indicate that about 50% of patients discontinue statin therapy one year after initiation (Alvarez-Jimenez et al., 2024). Digital health technologies, including wearable fitness trackers, mobile applications, and telemedicine platforms, offer promising solutions to improve patient engagement and monitor adherence in real-time. However, disparities in healthcare access remain, with CHD prevalence disproportionately higher in low-income communities and among ethnic minority groups (Bauser-Heaton et al., 2022). Addressing these disparities requires targeted public health strategies, culturally tailored interventions, and improved access to community-based healthcare services.
Despite the successes of early detection and good modern therapy, primary care physicians continue to have great difficulty managing the risk factors of CHD control. A widespread effort to reduce smoking rates remains a chimaera for smokers. Likewise, the high prevalence of obesity in the UK exacerbates the risk of developing CHD and other related conditions (Haase et al., 2020). Psychological factors, socioeconomic constraints, lower health literacy and other lifestyle practices often resist such lifestyle changes, and patient adherence to prescribed regimens is usually low for various reasons. Patients who are prescribed any medication such as statin sometimes discontinue it in the form of side effects or due to the belief that there will be no immediate benefit, sup doses inpatient and outpatient without any worry of side effects. According to Arya et al. (2019), the fashion of evaluating the Transonic Technology for Future Cardiology can include a simple, unobtrusive measurement of blood flow, a left ventricular pressure measurement, and cardiac output determined by these measurements.
National and Local Guidelines for CHD Diagnosis and Management
National frameworks in the UK for the management of CHD include NICE NG185, the NHS Long Term Plan, and the British Heart Foundation (BHF) policy recommendations. The guidelines are prevented from occurring through primary care screening programs, lifestyle interventions and pharmacological management. In England, the NHS Health Check was introduced to detect such individuals and provide appropriate preventive strategies to prevent the development of CVD (Nakaishi et al., 2022). Nevertheless, disparities in the provision of healthcare persist, with studies showing that people immersed in lower socioeconomic environments are 20% exposed to a greater danger of mortality for CHD-related causes (Rosengren et al., 2019). Although these gaps have not been entirely closed locally through initiatives at the local level, such as community-led cardiovascular risk screening programs, these have proved effective in improving early detection and specialist care.
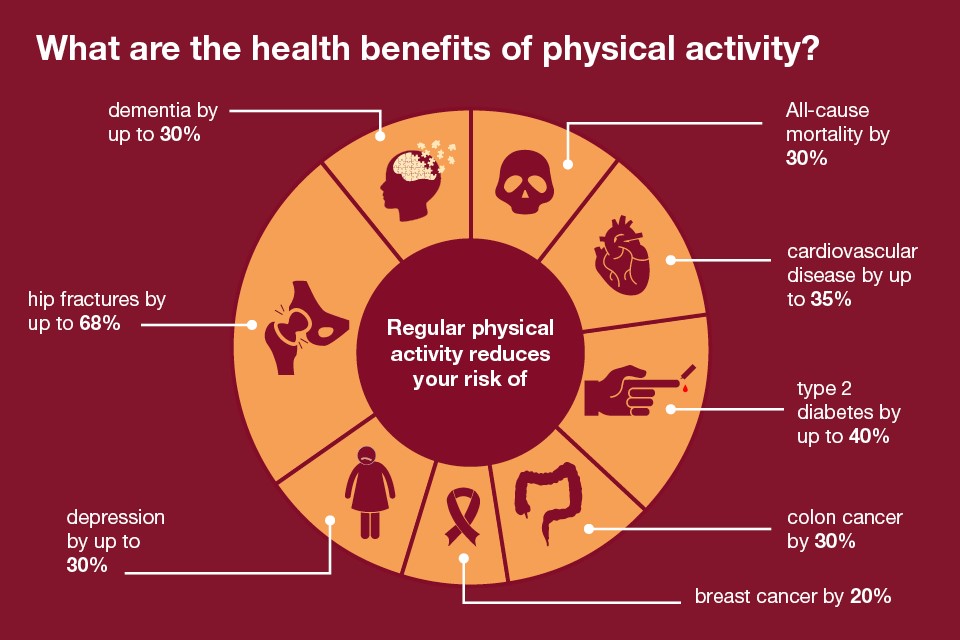
Figure 2: Physical activity: applying All Our Health
The British Heart Foundation (BHF) also gives policy recommendations that enable public health campaigns to proscribe CHD's dangers, including smoking, poor eating regimens, and physical inactivity (Public Health England, 2019). The BHF notes that people who suffer from chronic stress, anxiety and depression are at risk of CHD, something that it acknowledges is important for cardiac care. As per their guidelines, they stress these individuals’ guidelines suggest using comprehensive lifestyle interventions such as smoking cessation programs and adapted physical activity regimens. It is clear, however, that one key statistic of these guidelines being followed is that almost 37% of adults in the UK do not reach the recommended levels of physical activity, which is a major contributor to the problem of CHD (Office for Health Improvement and Disparities, 2022). The BHF recommends methods of community-based intervention and increased access to such health professionals in underserved areas to curb some of these lifestyle risk factors.
Meanwhile, local initiatives for CHD care support the empowerment of national frameworks for CHD care and bridging healthcare gaps, which also support equitable management of CHD. Some examples are community-led cardiovascular risk screening programs increasingly implemented in deprived areas. These programs aim to track people at high risk of developing CHD through local health services or community settings so that they can access screening and preventive care for whom they may not usually access formal health services (Ndejjo et al., 2021). The evidence is that these local initiatives matter, so early detection, reduced hospitalization, and other things caused by CHD complications should go down and up. Despite that, there are challenges because people from lower socioeconomic groups are more predisposed to CHD and face many more barriers to accessing care (Schultz et al., 2018). The data from Public Health England also reveals people from the most deprived areas are twice as likely to have a heart attack as those from more affluent areas.
Pharmacological and Non-Pharmacological Approaches
At present, Pharmacologic treatment remains a mainstay of CHD management: statins (at 20–40 mg daily), reduced LDL, beta-blockers (bisoprolol 2.5–10 mg daily), reduced myocardial oxygen demand and ACE inhibitors (ramipril 5–10 mg daily), improve endothelial function. Patients at high risk for thrombosis are usually given antiplatelet therapy, for example,e aspirin 75mg daily. Besides pharmacotherapy, preventive disease progression involves lifestyle modifications (Ojangba et al., 2023). Advice from national dietary recommendations is to consume less than 6g of salt per day, eat more fibre, and get moderately moderate exercise every 150 minutes per week.
Pharmacological and lifestyle adjustments manage CHD. The pharmacological approach focuses on medications, such as statins, which reduce harmful cholesterol levels; beta-blockers, which reduce heart load work; and ACE inhibitors, which support vascular health (Feingold & Grunfeld, 2024). They also suggest antiplatelet therapy using low-dose aspirin to prevent blood clot formation in the high-risk group. Structured cardiac rehabilitation programs, including physical exercise, nutrition counselling, and psychological support, have been implicated in improving the long-term stay of patients.
Reflection on Best Practices and Ethical Considerations
Clinical expertise and interventions play only a tiny part in effective cardiovascular care and entrust us with many essential ethical and professional responsibilities that impact the patient experience (Weidmann-Hügle & Monteverde, 2022). In the UK, fundamental principles in healthcare are patient confidentiality, informed consent, and shared decision-making, and healthcare professionals must abide by these. It ensures that care plans score well medically and fit the individuals’ preferences, personal values, and cultural beliefs. As per the view of Légaré et al. (2019), shared decision-making is becoming increasingly understood as essential, with the figure depicting that 60-70 per cent of patients feel more confident about the choice of treatment when utilised in the decision-making process. According to the situation, ethical dilemmas occur when patients won’t accept treatments or can not follow the treatment regimen as prescribed. These are the sorts of cases in which healthcare professionals are responsible for balancing respect for patient autonomy with the requirement to do good (beneficence). These scenarios are complex, and only transparent and empathetic communication will allow you to navigate them effectively so that the patient understands the options available and the potential consequences of choosing any option.
Non-adherence is a serious ethical problem that can have dire consequences for patient health in cardiovascular care (van der Laan et al., 2019). Chronic cardiovascular disease multiple studies show that up to 50 per cent of patients prescribed medication and lifestyle modifications are non-adherent to the regimens, contributing towards worsening of health risks. For patients to adhere to the treatment, healthcare providers should adopt several strategies, namely behavioural interventions, tailored care plans, and motivational interviewing techniques (Bischof et al., 2021). These approaches ensure that patients get informed and supported to make choices suitable to the interests of their health.
Personal Reflection on My Learning Journey
From reading this case study about the management of coronary heart disease (CHD), I have learned more about the pathophysiology of CHD and gained further insight into patient casework. The exploration of the potential host risk factors such as hypertension, hyperlipidaemia, obesity and smoking has increased my knowledge of the underlying causes of CVD as well as the importance of early detection and risk assessment. The emphasis has been put on proactive screening, lifestyle modifications, and pharmacological interventions in CHD management, as well as the reduction of the burden according to national guidelines such as the NHS Long Term Plan and NICE NG185 (NICE, 2020). The multidisciplinary approach to care has opened up my view of healthcare as a collaborative process, where each member brings a part to the whole and thus develops a care plan that represents the patient’s values and socioeconomic status. Secondly, I have gained a clearer understanding of the problems that involve patient adherence, especially to lifestyle changes and medication, and the use of behavioural change models to overcome all these challenges. In summary, this experience has enlightened me to a greater degree on cardiovascular healthcare, and it has brought home the value and need to continue to reflect and update my professional skills to provide improved patient care.
Conclusion
CHD represents a significant public health challenge in the UK and requires comprehensive risk assessment, intervention, and interprofessional working. Given the complexity of CHD management, the case study emphasizes that national guidelines and pharmacological and non-pharmaceutical strategies are essential for ethical considerations to maximize the prognosis of patients with CHD. Although progress has been made in lowering CVD mortality, there is still room for further work on preventive measures, healthcare delivery inequalities, and digital health representation in regular cardiovascular care. Improving long-term cardiovascular health in the UK will require a patient-centred approach supported by strong public health and community-based interventions.
References
- Afik, A., Nursalam, N., Sufyanti, A. Y., & Fikriana, R. (2022). Effect of Nurse-Led Program in Coronary Heart Diseases Patients: A Systematic Review. Open Access Macedonian Journal of Medical Sciences, 9(T5), 109–114. https://doi.org/10.3889/oamjms.2021.7861
- Alvarez-Jimenez, L., Morales-Palomo, F., Moreno-Cabañas, A., Mora-Gonzalez, D., Del, M., & Mora-Rodriguez, R. (2024). Time-Course Atherogenic Blood Lipid Response to Statin Discontinuation in Dyslipidemic Adults. Nutrition Metabolism and Cardiovascular Diseases. https://doi.org/10.1016/j.numecd.2024.05.021
- Arya, V., Kobe, J., Mishra, N., Al-Moustadi, W., Nates, W., & Kumar, B. (2019). Cardiac output monitoring: Technology and choice. Annals of Cardiac Anaesthesia, 22(1), 6. https://doi.org/10.4103/aca.aca_41_18
- Bauser-Heaton, H., Aggarwal, V., Graziano, J. H., R. Allen Ligon, Keeshan, B. C., Stapleton, G., Sutton, N. J., Fleming, G. A., Howaida El-Said, Dong, D., & Ing, F. F. (2022). Health Care Disparities in Congenital Cardiology: Considerations Through the Lens of an Interventional Cardiologist. 1(5), 100388–100388. https://doi.org/10.1016/j.jscai.2022.100388
- Bischof, G., Bischof, A., & Rumpf, H.-J. (2021). Motivational Interviewing: an Evidence-Based Approach for Use in Medical Practice. Deutsches Aerzteblatt Online, 118(7), 109–115. https://doi.org/10.3238/arztebl.m2021.0014
- Ewelina Młynarska, Czarnik, W., Piotr Fularski, Hajdys, J., Majchrowicz, G., Stabrawa, M., Rysz, J., & Franczyk, B. (2024). From Atherosclerotic Plaque to Myocardial Infarction—The Leading Cause of Coronary Artery Occlusion. International Journal of Molecular Sciences, 25(13), 7295–7295. https://doi.org/10.3390/ijms25137295
- Feingold, K. R., & Grunfeld, C. (2024). Cholesterol Lowering Drugs. Nih.gov; MDText.com, Inc. https://www.ncbi.nlm.nih.gov/books/NBK395573/
- Haase, C. L., Eriksen, K. T., Lopes, S., Satylganova, A., Schnecke, V., & McEwan, P. (2020). Body mass index and risk of obesity‐related conditions in a cohort of 2.9 million people: Evidence from a UK primary care database. Obesity Science & Practice, 7(2). https://doi.org/10.1002/osp4.474
- Hamrahian, S. M., Maarouf, O. H., & Fülöp, T. (2022). A Critical Review of Medication Adherence in Hypertension: Barriers and Facilitators Clinicians Should Consider. Patient Preference and Adherence, Volume 16(16), 2749–2757. https://doi.org/10.2147/ppa.s368784
- Légaré, F., Adekpedjou, R., Stacey, D., Turcotte, S., Kryworuchko, J., Graham, I. D., Lyddiatt, A., Politi, M. C., Thomson, R., Elwyn, G., & Donner-Banzhoff, N. (2019). Interventions for Increasing the Use of Shared Decision Making by Healthcare Professionals. Cochrane Database of Systematic Reviews, 7(7). https://doi.org/10.1002/14651858.cd006732.pub4
- Mehta, K. (2024, June 5). South Asians almost twice as likely to develop coronary heart disease than White Europeans. Www.bhf.org.uk. https://www.bhf.org.uk/what-we-do/news-from-the-bhf/news-archive/2024/june/south-asians-almost-twice-as-likely-to-develop-coronary-heart-disease-than-white-europeans
- Nakaishi, L., Sugden, S. G., & Merlo, G. (2022). Primary Care at the Intersection of Lifestyle Interventions and Unhealthy Substance Use. American Journal of Lifestyle Medicine, 155982762211110. https://doi.org/10.1177/15598276221111047
- Ndejjo, R., Hassen, H. Y., Wanyenze, R. K., Musoke, D., Nuwaha, F., Abrams, S., Bastiaens, H., & Musinguzi, G. (2021). Community-Based Interventions for Cardiovascular Disease Prevention in Low-and Middle-Income Countries: A Systematic Review. Public Health Reviews, 42(1604018). https://doi.org/10.3389/phrs.2021.1604018
- NHS England. (2014). Five Year Forward View. In NHS England. NHS England. https://www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf
- NICE. (2020, November 18). Overview | Acute coronary syndromes | Guidance | NICE. Www.nice.org.uk. https://www.nice.org.uk/Guidance/NG185
- Nichol, J. R., Nelson, G., & Sundjaja, J. H. (2024, April 30). Medical History. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK534249/
- Office for Health Improvement & Disparities. (2022, April 5). Smoking and tobacco: Applying All Our Health. GOV.UK. https://www.gov.uk/government/publications/smoking-and-tobacco-applying-all-our-health/smoking-and-tobacco-applying-all-our-health
- Office for Health Improvement and Disparities. (2022, March 10). Physical activity: Applying All Our Health. GOV.UK. https://www.gov.uk/government/publications/physical-activity-applying-all-our-health/physical-activity-applying-all-our-health
- Ojangba, T., Boamah, S., Miao, Y., Guo, X., Fen, Y., Agboyibor, C., Yuan, J., & Dong, W. (2023). Comprehensive effects of lifestyle reform, adherence, and related factors on hypertension control: A review. The Journal of Clinical Hypertension, 25(6). https://doi.org/10.1111/jch.14653
- Parreira, P., Santos-Costa, P., Neri, M., Marques, A., Queirós, P., & Salgueiro-Oliveira, A. (2021). Work methods for nursing care delivery. International Journal of Environmental Research and Public Health, 18(4), 2088. https://doi.org/10.3390/ijerph18042088
- Powell-Wiley, T. M., Poirier, P., Burke, L. E., Després, J.-P., Gordon-Larsen, P., Lavie, C. J., Lear, S. A., Ndumele, C. E., Neeland, I. J., Sanders, P., & St-Onge, M.-P. (2021). Obesity and Cardiovascular disease: a Scientific Statement from the American Heart Association. Circulation, 143(21), 984–1010. https://doi.org/10.1161/cir.0000000000000973
- Public Health England. (2019, February 14). Health matters: preventing cardiovascular disease. Gov.UK. https://www.gov.uk/government/publications/health-matters-preventing-cardiovascular-disease/health-matters-preventing-cardiovascular-disease
- Pursnani, S., & Merchant, M. (2020). South Asian ethnicity as a risk factor for coronary heart disease. Atherosclerosis, 315, 126–130. https://doi.org/10.1016/j.atherosclerosis.2020.10.007
- Rosengren, A., Smyth, A., Rangarajan, S., Ramasundarahettige, C., Bangdiwala, S. I., AlHabib, K. F., Avezum, A., Bengtsson Boström, K., Chifamba, J., Gulec, S., Gupta, R., Igumbor, E. U., Iqbal, R., Ismail, N., Joseph, P., Kaur, M., Khatib, R., Kruger, I. M., Lamelas, P., & Lanas, F. (2019). Socioeconomic status and risk of cardiovascular disease in 20 low-income, middle-income, and high-income countries: the Prospective Urban Rural Epidemiologic (PURE) study. The Lancet Global Health, 7(6), e748–e760. https://doi.org/10.1016/s2214-109x(19)30045-2
- Schultz, W. M., Kelli, H. M., Lisko, J. C., Varghese, T., Shen, J., Sandesara, P., Quyyumi, A. A., Taylor, H. A., Gulati, M., Harold, J. G., Mieres, J. H., Ferdinand, K. C., Mensah, G. A., & Sperling, L. S. (2018). Socioeconomic Status and Cardiovascular Outcomes: Challenges and Interventions. Circulation, 137(20), 2166–2178. https://doi.org/10.1161/circulationaha.117.029652
- Thibaut, F. (2018). Body-mind interaction in psychiatry. Dialogues in Clinical Neuroscience, 20(1). https://doi.org/10.31887/dcns.2018.20.1
- Tidy, C. (2022, July 22). Epidemiology of Coronary Heart Disease. Patient.info. https://patient.info/doctor/epidemiology-of-coronary-heart-disease
- Toukhsati, S., Jaarsma, T., Babu, A., Driscoll, A., & Hare, D. (2019). Self-Care Interventions That Reduce Hospital Readmissions in Patients With Heart Failure; Towards the Identification of Change Agents. Clinical Medicine Insights: Cardiology, 13(1), 117954681985685. https://doi.org/10.1177/1179546819856855
- van der Laan, D. M., Elders, P. J. M., Boons, C. C. L. M., Nijpels, G., & Hugtenburg, J. G. (2019). Factors Associated With Nonadherence to Cardiovascular Medications. The Journal of Cardiovascular Nursing, 34(4), 344–352. https://doi.org/10.1097/JCN.0000000000000582
- Weidmann-Hügle, T., & Monteverde, S. (2022). Clinical Ethics Consultation in Chronic Illness: Challenging Epistemic Injustice Through Epistemic Modesty. HEC Forum. https://doi.org/10.1007/s10730-022-09494-8

