- Introduction - Impact of antibiotic resistance on the management of recurrent urinary tract infections.
- Discussion
- Challenges in antibiotic treatments
- The use of alternative therapies
- Healthcare systems implications
- Conclusion
- Presentation
- Slide 1: Title
- Slide 2: Introduction
- Slide 3: Background
- Slide 4: Hypothesis
- Slide 5: Methods
- Slide 6: Results
- Slide 7: Results
- Slide 8: Discussion
- Slide 9: Discussion
- Slide 10: Conclusion
Introduction - Impact of antibiotic resistance on the management of recurrent urinary tract infections.
Urinary tract infections (UTIs) are considered among the most widespread bacterial infections that affect millions of individuals across the world including women. rUTIs specifically those who have had at least two or more times within the next six months or three times within one year constitute a tough optimization challenge. Recently, antibiotics have often been taken as the primary treatment of rUTIs. Nevertheless, the number of antibiotic-resistant uropathogens raise concerns on the effectiveness of antibiotics. The WHO has declared antibiotic resistance as a major global threat and Escherichia coli (E. coli) that is resistant to multiple antibiotics is the most common UTI-pathogen. This paper aims at discussing antibiotic resistance concerning rUTI to understand the challenges in treatment, the need for other therapy approaches and the impact in the general health sector.
Discussion
Challenges in antibiotic treatments
The spread of antibiotic resistance thus makes it easier for bacteria to develop resistance to the antibiotics thus complicating the treatment of recurrent urinary tract infections (rUTIs). Some bacteria are resistant to known antibiotics and cause urinary tract infections or UTI for short. Among them, ESBL-producing Escherichia coli (E. coli) is one significant issue because the bacteria have a longer spectrum of β-lactamase that deactivates broader categories of antibiotic drugs. They can decompose important antibiotics and this makes the treatment to be of no effect. Another severe threat is carbapenem-resistant Enterobacteriaceae (CRE), which are resistant to some of the most potent antibiotics that are available in the market (Kwok et al. 2022). Most of the first-line antimicrobial agents such as fluoroquinolones and beta-lactam have diminished efficiency against rUTIs. These were some of the most effective in the treatment of infections, but have become ineffective due to emergence of resistance.
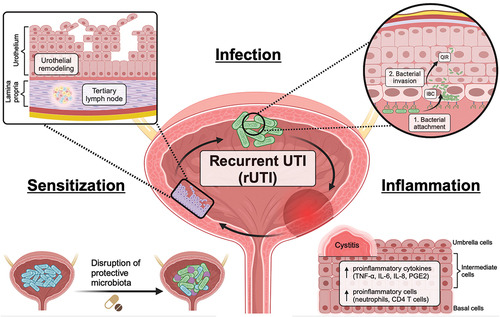
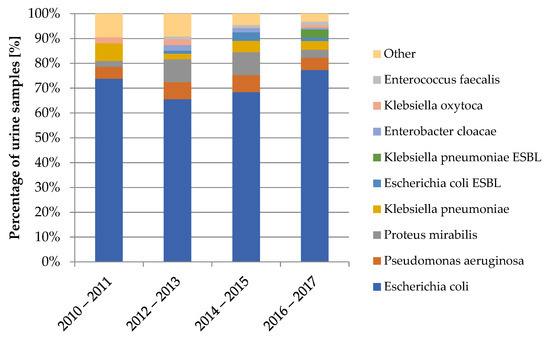
Figure 1: Overcoming challenges in UTI
This result shows that in the case where antibiotics are not effective, infections take a long to treat. This is could be quite cumbersome to the patients and more so if complications arise such as pyelonephritis which is a kidney infection and sepsis, which is a bloodstream infection. The reader might need a more potent antibiotic capable of eradicating all the bacterial, but these come with additional effects and can be too costly. Patients sometimes require being admitted and given intravenous (IV) antibiotics as a type of treatment plan. Some of the main factors contributing to development of resistance include misuse through inept prescription and over prescription of drugs (Simoni et al. 2024). However, this also casts a problem to the bacteria making it develop a resistance far much faster. If antibiotics are used frequently then, specific bacteria species will survive and instead pose a greater threat in the future infections.
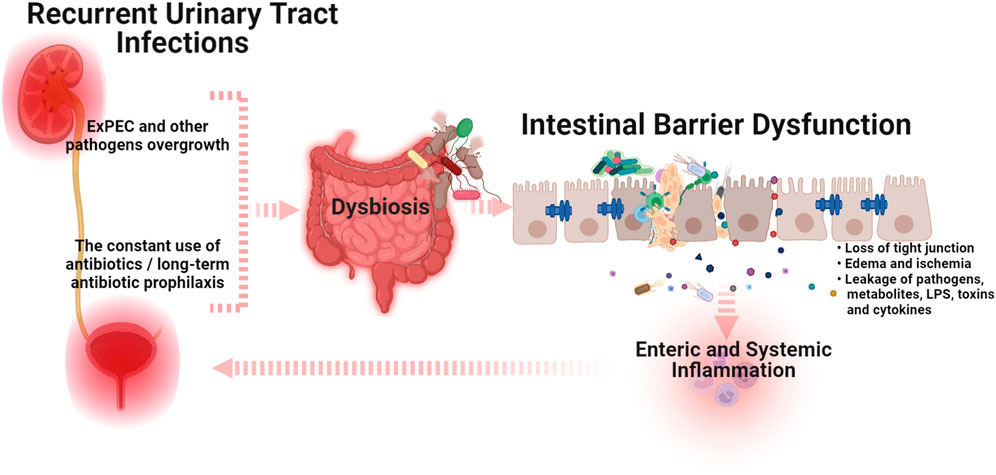
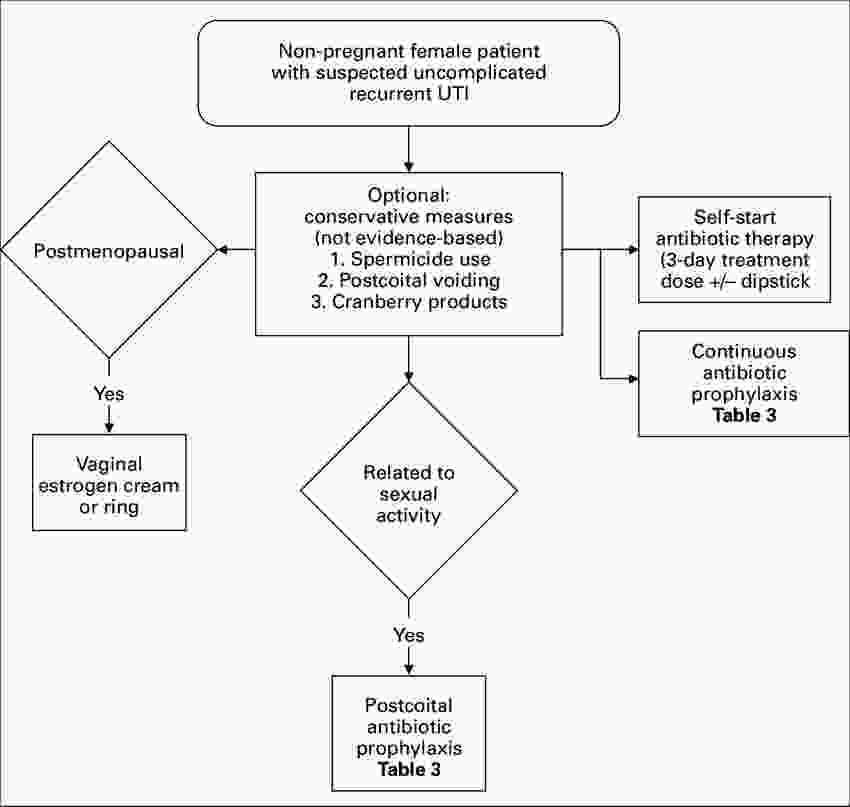
The use of alternative therapies
Since the effectiveness of antibiotics is declining scientists and physicians are in search of other strategies for handling rUTIs. The following are the possible remedies that people are looking forward to instead of antibiotics.
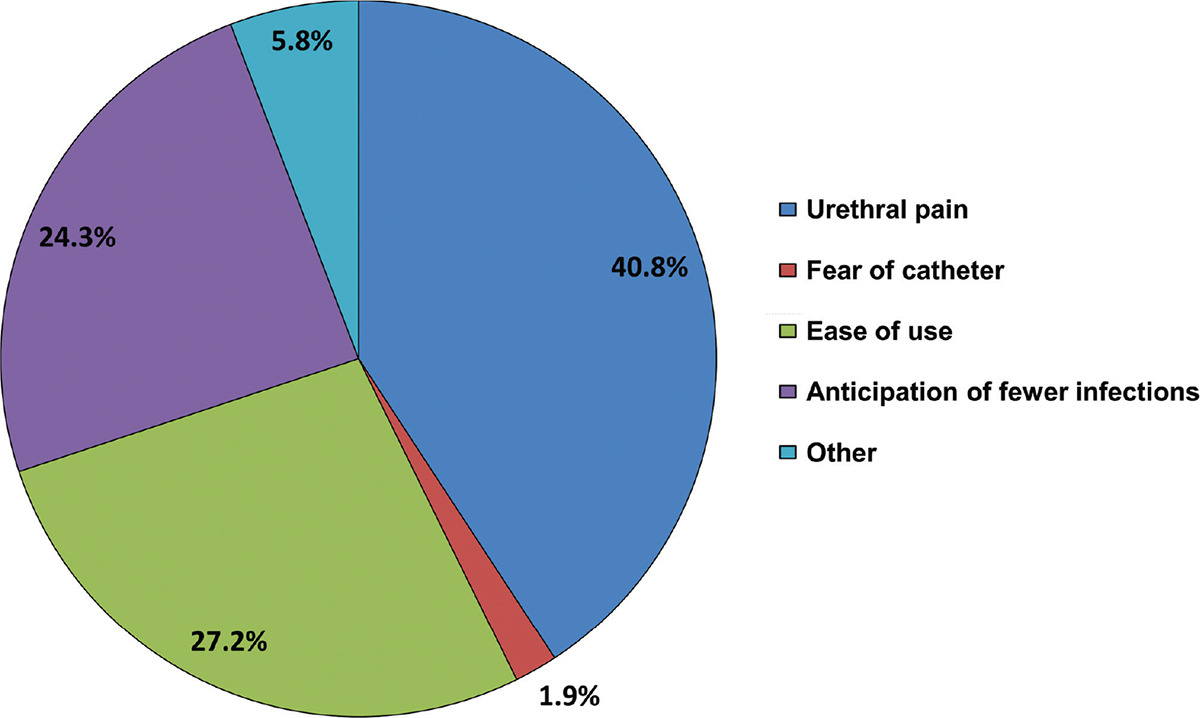
Intravesical Therapy: This is the process where antibiotics or antiseptics are introduced into the bladder through a catheter. This therapy places the medication directly to the affected area, an aspect that puts it at an advantage in getting round some of the challenges associated with antibiotic resistance seen when they are taken orally. To a large extent it is particularly useful in cases of chronic or relapse of infections.
Probiotics: These are friendly bacteria that assist the body to work in the right way that can be expected. Strains of Lactobacillus are normally found in the vagina or the urinary area and may outcompete pathogenic organisms for survival (Harding et al. 2022). According to some researchers, the consumption of probiotics may be in the form of pill supplements or products that contain probiotics like yogurts may be effective in preventing rUTIs.
Cranberry Juice Concentrate: Their effectiveness is derived from products containing proanthocyanidins that prevent bacteria from adherence to bladder lining. Depending on the product that is taken, cranberry results to inhibit bacterial attachment therefore reducing the overall instances of infections.
Bacteriophage Therapy: This is one of the newly developing techniques that involves using viruses known as bacteriophages to attack and infect bacteria. In contrast to antibiotics, bacteriophages are harmless to the useful bacteria (Jalil MB et al. 2022). Several studies were conducted and have yielded some promising results but further research had to be done to warrant its use and prescription for rUTIs.
As much as these therapies are encouraging, they are still considered to be complementary therapies. But they may become relevant choices in the future as the levels and intensity of antibiotic resistance goes up.
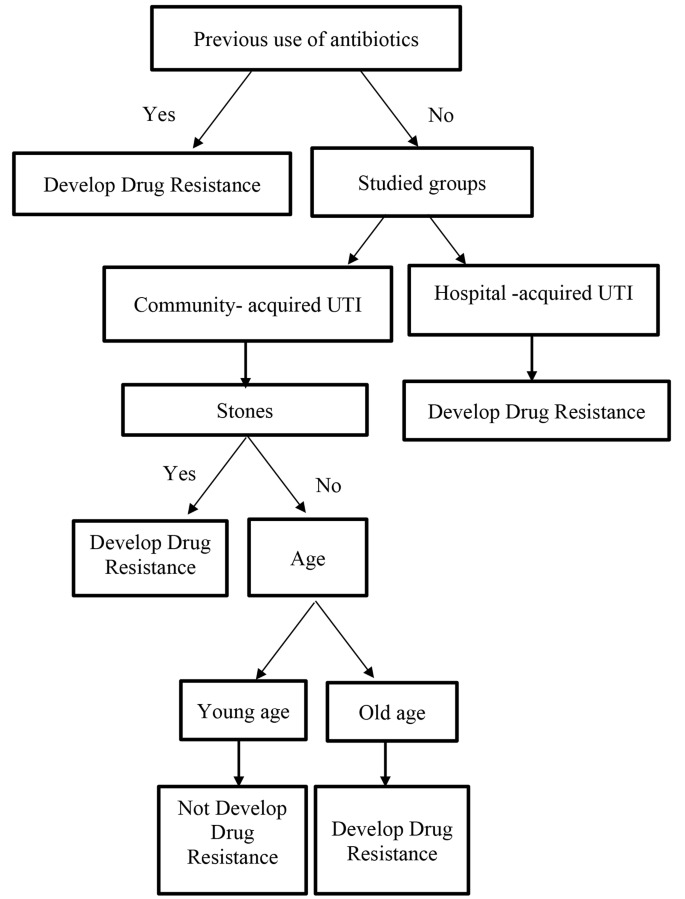
Figure 2: Trends and predictors of antimicrobial resistance
Healthcare systems implications
Non-extreme antibiotic-resistant rUTIs are not only an issue in terms of the individual patient. They impose additional burden to the health care facilities due to the rise in demand for hospital health care, more tests, and higher potency medications. Every time antibiotics are administered and fail, patients will be taken longer days in illness. This entitles them to more doctor appointment, more test, and potential hospitalizations. Some of them may require IV antibiotics which cost more and needs strict medical supervision (Karunarathna et al. 2024). These factors lead to an addition in the costs of healthcare for not only the patients but also to the hospitals. Another concern is what has been referred to as the ‘last’ line of antibiotics such as carbapenems. These medications have to be prescribed when other forms of medication are not effective. Although due to the growing resistance against them, they are being applied more frequently. Carbapenem's use increases the appearance of the stronger generation of bacteria, and antibiotics that can combat them in the future are extremely scarce.
To prevent further increase in the levels of antibiotic resistance in healthcare settings, there is a need for the implementation of measures that encourage prudent use of antibiotics. In this case, there are programs such as antimicrobial stewardship that makes it compulsory to use antibiotics only when necessary. Sanitisation is also crucial given that the virus is very much present and active currently (Mancuso et al. 2023). In general, the presence of resistant bacteria in hospitals and clinics should be controlled through effective hygiene practices. Some of them are hand washing, instrument sterilization and proper isolation of any infectious individual that may be in the medical facility. The best control of rUTIs and the effects of antibiotic resistance can be achieved by using smart antibiotic prescription and application, employing other effective methods and having enhanced infection control sentences in the healthcare systems.
Achieve excellence with our trusted Online Assignment Help service! From essays to dissertations, we deliver professional writing assistance that combines expertise, reliability, and commitment to your academic success.
Conclusion
Over the course of the past years, positive findings of antibiotic resistance have made the UTI recurrent and difficult to treat hence more patients resort to other forms of therapy. Hence, there is a need to embrace antimicrobial stewardship, patient education, and research in efficient ways of combating resistant rUTIs. As a result, future research should look at developing other forms of treatment besides antibacterial and finding new methods to fight the resistance. It is evident that by using a complex approach, rUTIs can be well managed for healthcare professionals, with concurrent reduction of the ramifications of antibiotic resistance in the long run.
Presentation
Slide 1: Title
Slide 2: Introduction
- Antibiotic resistance complicated UTI treatment
- New rUTIs are increasing in frequency
- Feasibility of adopting different approaches in rUTIs control
S.N: The bacterial provided resistance to antibiotics has become one of the major challenges in the globe. It impacts the treatment of several infections such as the urinary tract infections (UTIs). They are prevalent in women and are among the frequently treated infections in women and in the general population. About 20-50% of them suffer from rUTIs, which means the girls and women continue to get infected many times and need antibiotics each time. In this presentation, the topic of Focus will be on understanding management of antibiotic resistance in rUTI and new therapies that can be available to manage this problem.
Slide 3: Background
- UTIs are a condition that results from bacteria invading or penetrating the urethra.
- Resistant strains reduce antibiotic effectiveness
- Urgent need for alternative treatments
S.N: It is seen that UTIs are produced when bacteria enter into the body through the urethra and then get settled in the bladder. The majority of UTIs are treated using antibiotics, but uncontrolled use led to emergence of antibiotic resistance. However, one of the obstacles, which has recently emerged as a difficult problem, is that bacteria become increasingly resistant to antibiotics (Okeke et al. 2024). Several strains of bacteria like the extended-spectrum beta-lactamase (ESBL)-producing E. coli cannot be treated with conventional antibiotics, particularly, penicillin’s and cephalosporins. This contributes to extended hospitalization, increased expense, and development of severe kidney infection, specifically pyelonephritis or bloodstream infection, specifically sepsis.
Slide 4: Hypothesis
- The elevated rates further deteriorate the treatment outcomes of rUTI
- Standard antibiotics losing effectiveness rapidly
- It thus emerged that there is a need for new therapies as well as stewardship
S.N: If things progress as they are, the recurrent UTI cases will be hard to treat because of growing antibiotic resistance. Essential drugs will be less effective, the patients will suffer for longer periods, as well as experience more severe cases of the disease (Bavanandan, and Keita, 2023). Bacterial resistance will only be checked if there are more changes in use of antibiotics and modern infection control.
Slide 5: Methods
- The qualitative analysis on current literatures.
- Emphasizing on paths of resistance and rates of success
- Identified potential alternative treatment options
S.N: This is done drawing from recent studies on rUTI and its treatment to identify the emerging issues on antibiotic resistance. To gather data, only the research articles published from 2020 and the subsequent years were taken into consideration from the peer-reviewed publications only. Common antibiotic-resistant bacteria in UTIs and their prevalence worldwide. This article is a good example of the effectiveness of the standard antibiotics and also the failure rates because of resistance (Rostkowska et al. 2021). Other adjunct therapies still under development in clinical trials, which give hope of non-antibiotic tactics. The purpose therefore was to determine the effects of resistance and also find out what other solutions can be offered and employed in implementing a change.
Slide 6: Results
- More than 30% of the E. coli strains isolated are resistant
- ESBL-producing bacteria increase hospital admissions
- The therapies appear to have the possibility that is therapeutic for treatment
S.N: There is the emergence of antibiotic resistance which hampers the efficiency of treatment for rUTI. ESBL-producing bacteria lead to higher hospital admissions and longer treatment durations. The cases of last-line drugs such as carbapenems are on the rise owing to the several side effects that are associated with them and they may also cause further development of resistance strains (Stracy et al. 2022). There is scientific evidence that supports the use of non-antibiotic remedies like probiotics and formulations containing cranberry extracts and alleges that they are effective in stopping infections but more studies are needed. It continues to make the costs of healthcare rise, lower the rate of treatment and treatment access, hence making it necessary to look for better ways to address the problem.
Slide 7: Results
- Intravesical therapy bypasses resistance issues
- Bacteriophage therapy is an upcoming method that has a very good potential
- Nanotechnology may enhance drug effectiveness
S.N: There is more emphasis on the various other treatments since conventional antibiotics have proven to be ineffective and have higher chances of resistance. Intravesical delivery of antibiotics allows the antibiotics to be placed directly into the bladder, thus, they will not be affected by systemic resistance and have minimal side effects. Thus, nanotechnology can enhance cancer drugs, deliver drugs more precisely, and get past the wall of infection to target tough bacteria cells and may lessen the quantity of antibiotics required. However, it is notable that despite these treatments having a certain effectiveness, studies and approvals are required more so for these treatments to be fashioned as standard ones.
Slide 8: Discussion
- Resistant UTIs contribute to both the length of hospitalization and costs
- Misuse of the medication makes the resistance levels to go high
- The study affirms that more research is needed for effective solutions
S.N: Some UTIs are resistant to antibiotics since the drugs are utilized frequently and improperly. This enhances the failures of treatment, hospitalization, as well as the general overall healthcare expenditures, making the infection difficult to handle. Hospitals do not efficiently manage hard-to-killing pathogen-associated infections especially for patients who are immune-compromised, such as the geriatrics or those with chronic diseases (Sher et al. 2024). Severity of illnesses, longer hospital stays, an increased susceptibility of getting complications, more incidences of severe infections such as sepsis. More specifically, promising approaches for treatment and effective infection control should be to be established hence the need for research.
Slide 9: Discussion
- Therapies are not fully adopted yet by most insurance companies.
- The utilization of probiotics and cranberry extracts requires validation.
- It is crucial that existing policies do not hamper the efforts towards the prevention of resistance.
S.N: The use of the other therapies might help to minimize the use of the antibiotics and thus make little impact on resistance. Nonetheless, they are not applied in the clinical setting to the fullest extent possible since there may be a lack of evidence or there are regulatory issues. Probiotics and cranberry extracts have promising benefits during prevention and may under certain circumstances be effective in stopping the bacteria growth solely depending on the patient and type of bacteria. Bacteriophage therapy and nanotechnology are attractive but still costly and still in the experimental stage with several precautions to observe (Zhu et al. 2021). Policies on healthcare ought to enhance antibiotic stewardship measures, such as the provision of better measures of infection control, patient enlightenment, and stringent prescription of antibiotics.
Slide 10: Conclusion
- This makes rUTIs less treatable since some of their characteristics are resistant
- New treatments offer promising alternatives
- Responsible antibiotic use is crucial
S.N: Antibiotic resistance has become a challenge in the treatment of rUTIs and this makes the infection to persist for longer durations and results in more expensive health-related effects. Newer modes of treatment in the management of them are, Probiotics, Bacteriophage therapy, Intravesical antibiotics. To avoid such a situation, the healthcare providers must ensure that they use antibiotics judiciously so that they can remain useful to other generations of patients. Taking measures to make the public know ways of preventing UTIs and the spread of the resistant bacterium is an important step towards minimizing their occurrence.
Reference List
Journals
- Aggarwal N, Leslie SW. Recurrent Urinary Tract Infections. 2025 Jan 20. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan–. PMID: 32491411.
- Bavanandan S, Keita N. Urinary Tract Infection Prevention and Treatment. Semin Nephrol. 2023 Sep;43(5):151468. doi: 10.1016/j.semnephrol.2023.151468. Epub 2024 Feb 24. PMID: 38403525.
- Czajkowski K, Broś-Konopielko M, Teliga-Czajkowska J. Urinary tract infection in women. Prz Menopauzalny. 2021 Apr;20(1):40-47. doi: 10.5114/pm.2021.105382. Epub 2021 Apr 21. PMID: 33935619; PMCID: PMC8077804.
- Harding C, Mossop H, Homer T, Chadwick T, King W, Carnell S, Lecouturier J, Abouhajar A, Vale L, Watson G, Forbes R, Currer S, Pickard R, Eardley I, Pearce I, Thiruchelvam N, Guerrero K, Walton K, Hussain Z, Lazarowicz H, Ali A. Alternative to prophylactic antibiotics for the treatment of recurrent urinary tract infections in women: multicentre, open label, randomised, non-inferiority trial. BMJ. 2022 Mar 9;376:e068229. doi: 10.1136/bmj-2021-0068229. PMID: 35264408; PMCID: PMC8905684.
- Jalil MB, Al Atbee MYN. The prevalence of multiple drug resistance Escherichia coli and Klebsiella pneumoniae isolated from patients with urinary tract infections. J Clin Lab Anal. 2022 Sep;36(9):e24619. doi: 10.1002/jcla.24619. Epub 2022 Jul 23. PMID: 35870190; PMCID: PMC9459318.
- Karunarathna, I., Gunasena, P., Gunathilake, S. and De Alvis, K., 2024. Antibiotic resistance and gentamicin: Current trends and clinical implications.
- Kwok M, McGeorge S, Mayer-Coverdale J, Graves B, Paterson DL, Harris PNA, Esler R, Dowling C, Britton S, Roberts MJ. Guideline of guidelines: management of recurrent urinary tract infections in women. BJU Int. 2022 Nov;130 Suppl 3(Suppl 3):11-22. doi: 10.1111/bju.15756. Epub 2022 May 17. PMID: 35579121; PMCID: PMC9790742.
- Mancuso G, Midiri A, Gerace E, Marra M, Zummo S, Biondo C. Urinary Tract Infections: The Current Scenario and Future Prospects. Pathogens. 2023 Apr 20;12(4):623. doi: 10.3390/pathogens12040623. PMID: 37111509; PMCID: PMC10145414.
- Okeke IN, de Kraker MEA, Van Boeckel TP, Kumar CK, Schmitt H, Gales AC, Bertagnolio S, Sharland M, Laxminarayan R. The scope of the antimicrobial resistance challenge. Lancet. 2024 Jun 1;403(10442):2426-2438. doi: 10.1016/S0140-6736(24)00876-6. Epub 2024 May 23. Erratum in: Lancet. 2024 Sep 14;404(10457):1018. doi: 10.1016/S0140-6736(24)01879-8. PMID: 38797176.
- Pereira A, de Sousa T, Silva C, Igrejas G, Poeta P. Impact of Antimicrobial Resistance of Pseudomonas aeruginosa in Urine of Small Companion Animals in Global Context: Comprehensive Analysis. Vet Sci. 2025 Feb 11;12(2):157. doi: 10.3390/vetsci12020157. PMID: 40005917; PMCID: PMC11860736.
- Rostkowska OM, Międzybrodzki R, Miszewska-Szyszkowska D, Górski A, Durlik M. Treatment of recurrent urinary tract infections in a 60-year-old kidney transplant recipient. The use of phage therapy. Transpl Infect Dis. 2021 Feb;23(1):e13391. doi: 10.1111/tid.13391. Epub 2020 Jul 14. PMID: 32599666.
- Sher EK, Džidić-Krivić A, Sesar A, Farhat EK, Čeliković A, Beća-Zećo M, Pinjic E, Sher F. Current state and novel outlook on prevention and treatment of rising antibiotic resistance in urinary tract infections. Pharmacol Ther. 2024 Sep;261:108688. doi: 10.1016/j.pharmthera.2024.108688. Epub 2024 Jul 6. PMID: 38972453.
- Simoni A, Schwartz L, Junquera GY, Ching CB, Spencer JD. Current and emerging strategies to curb antibiotic-resistant urinary tract infections. Nat Rev Urol. 2024 Dec;21(12):707-722. doi: 10.1038/s41585-024-00877-9. Epub 2024 May 7. PMID: 38714857; PMCID: PMC11540872.
- Stracy, M., Snitser, O., Yelin, I., Amer, Y., Parizade, M., Katz, R., Rimler, G., Wolf, T., Herzel, E., Koren, G. and Kuint, J., 2022. Minimizing treatment-induced emergence of antibiotic resistance in bacterial infections. Science, 375(6583), pp.889-894.
- Zhu, H., Chen, Y., Hang, Y., Luo, H., Fang, X., Xiao, Y., Cao, X., Zou, S., Hu, X., Hu, L. and Zhong, Q., 2021. Impact of inappropriate empirical antibiotic treatment on clinical outcomes of urinary tract infections caused by Escherichia coli: a retrospective cohort study. Journal of global antimicrobial resistance, 26, pp.148-153.

